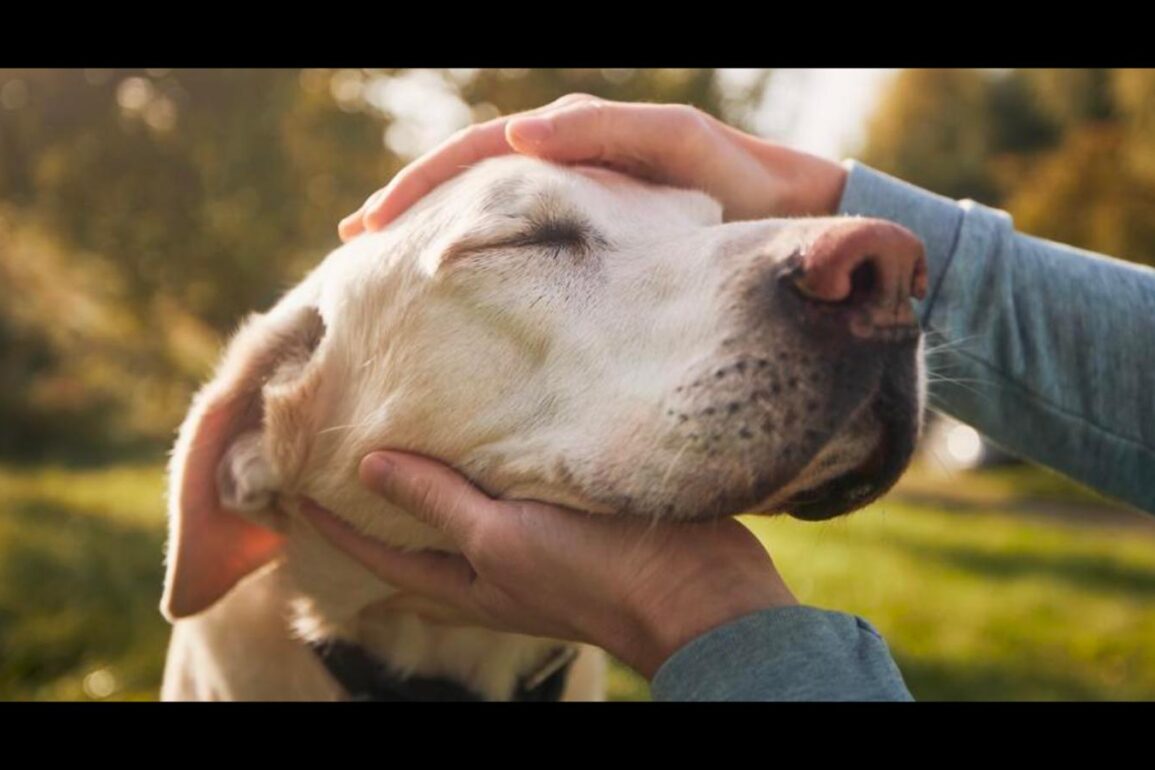
Welcome to Pet Peeves, a monthly series that aims to provide pet care solutions and expert advice for challenging scenarios that involve your beloved animal companions.
Anyone with a senior pet knows that seeing their dog or cat grow older is a privilege. But as your pet ages, in addition to seeing their fur turn adorably frosty, it’s likely you’ll witness some changes in their mobility, too. Perhaps they might start to hop out of bed a little less quickly for their morning walk, for example, or seem overall slower-paced than they were in their younger years.
“As pets age, the most common factors affecting their mobility include osteoarthritis, degenerative joint disease and muscle atrophy,” says Dr. Lisa Lippman, a veterinarian and director of virtual medicine at Bond Vet. “Other issues such as spinal problems, hip dysplasia and obesity can also contribute to decreased mobility. In some cases, neurological conditions or systemic diseases can further complicate mobility.”
To help you navigate dealing with an aging pet with mobility problems, I consulted three veterinarians for their advice on how to keep your older dog or cat as comfortable as possible during this phase of their life. While some degree of slowing down is inevitable, there are many ways to help mitigate your dog’s or cat’s aches and pains as they become less mobile—even if they are affected by any of the above issues as they get older. And as someone who recently adopted a 13-year-old dog (and who has lived with several senior cats and volunteers regularly at my local animal shelter), I’ve had my fair share of experience treating arthritis and learning how to identify signs of pain. From supplements and prescription medications to outfitting your home in a way that allows them to move around more easily, here’s how to be there for your aging pet.
Discuss Any Changes In Behavior With Your Veterinarian
While joint issues like osteoarthritis affect 20% of dogs older than one year, they affect 80% of dogs older than eight years, according to various studies. And it’s a similar story with cats: 60% of cats six years or older and 90% of cats over 12 can be diagnosed with osteoarthritis pain. “Signs of pain can be subtle and include changes in behavior, such as reluctance to move, hiding or decreased interest in favorite activities,” says Lippmann. “You might also notice changes in posture, such as stiffness when getting up, a reluctance to jump or walking more slowly.” Other indications of pain in dogs, she adds, can include licking or chewing at a specific joint, a decreased appetite or becoming irritable or withdrawn.
Cats, meanwhile, are especially masterful at hiding their pain, meaning it might not always be as obvious. “Pain can negatively impact cognitive function, sleep patterns, sensitivity to environmental stimuli and disrupt relationships with both humans and other household animals,” says Dr. Tracey Deiss, a veterinarian with animal-health company Zoetis who specializes in feline pain. “Cats tend to manifest osteoarthritis pain differently than dogs, often not showing the typical signs like limping and their ability to mask joint pain during exams.” That’s why it’s crucial to see your veterinarian regularly—especially if you notice any behavior changes.
Dr. Courtney Pierce, a veterinarian with Zoetis specializing in canine pain, notes that “many dogs do not get a diagnosis of osteoarthritis until the disease is quite progressed and significant pain is present.” This means it can make effective treatment much more challenging; it also underscores the importance of annual physical exams and other routine preventative measures. In addition, she stresses that vocalization (like crying, whimpering or whining) is not a common way for pets to communicate they’re experiencing pain, especially if it’s chronic, often making it difficult for dog guardians to identify.
Your veterinarian may recommend prescription medications like NSAIDs (non-steroidal anti-inflammatory drugs), gabapentin or injectables to help treat your pet’s particular issues and manage their pain. But just remember that what’s effective for some animals doesn’t always work for others, so you might wind up needing to go through a bit of trial and error. Physical therapy options may also be beneficial, such as hydrotherapy (underwater treadmill walking), massage, laser therapy, acupuncture and more.
Ensure They Maintain A Healthy Weight
Keeping your pet at a healthy weight is important throughout their life, but it’s particularly crucial as they get older, as unnecessary weight can put more pressure on their joints and affect their mobility. “Studies have shown that when pets are kept lean, the onset of osteoarthritis is delayed compared to those dogs that are overweight,” says Pierce.
Make sure they’re eating a balanced diet and have a caloric intake that’s appropriate for their ideal weight. “Diets formulated for joint health, especially those containing omega-3 fatty acids, can support joint function,” says Lippman, who recommends supplements like fish oil, glucosamine and green-lipped mussel. I’ve had good experiences using over-the-counter joint supplements like Movoflex and Dasaquin for my geriatric dog, but it’s always best to consult with your veterinarian for their recommendations before starting your pet on anything new. Additionally, there are plenty of dog food delivery services that you can customize to target your pet’s particular needs.
“As for exercise, regular but moderate activity is important—short, frequent walks rather than long ones, adjusted based on how your pet feels,” adds Lippman. “Avoid overexertion and always monitor for any signs of discomfort.” Pierce also advises gentle, consistent activity to keep joints flexible and muscles strong and suggests interactive play sessions that promote movement without over-stressing the joints.
Create A Comfortable Home Environment For Them
Unfortunately, there’s no cure for osteoarthritis, but there are plenty of steps you can take to ensure your home best accommodates your senior pet’s needs, whether they are dealing with arthritis or other joint issues. “Provide ramps to help them access favorite spots, ensure litter boxes have low sides for easy entry and offer soft bedding to cushion their joints,” suggests Deiss. You might also want to consider covering any hard flooring surfaces with rugs, runners or mats to help with traction.
For more recommendations, take a look at our list of the best dog ramps and the best orthopedic dog beds. I also use this large-breed dog stroller for my senior dog when we go on walks to the vet’s office; we walk for as long as she’s comfortable, and once she gets tired, she steps right up into it and we keep it moving. Plus, an elevated feeding station (I use this one from Trot Pets, which also comes with a slow-feeder bowl) can help them eat and drink more easily, so they don’t need to bend their head all the way down to the ground.
With cats, observe their behavior and consider whether they should have access to a cat tree; if they’re going through treatment and seem to be rehabilitating, “don’t allow your cat access to a cat tree until they are ready to jump from those heights,” says Deiss, who recommends gradually adding levels back as they progress.
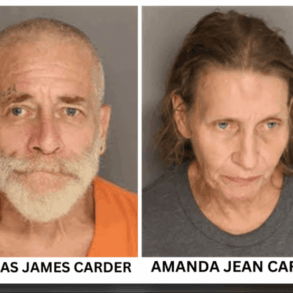
Meet The Experts
Lisa Lippman, DVM, is a New York-based veterinarian and director of virtual medicine at Bond Vet who earned her degree in veterinary medicine at Western University of Health Sciences. She also sits on the board of Animal Lighthouse Rescue, whose mission is to help the homeless dogs of Puerto Rico. She’s co-host of the podcast We Don’t Deserve Dogs and has been featured as a veterinary expert on Good Morning America, Dr. Oz, Inside Edition and more.
Courtney Pierce, DVM, MBA, is a Virginia-based small-animal veterinarian who earned her degree in veterinary medicine from North Carolina State University. She is the medical lead for canine pain at Zoetis and has special interests in surgery and pain management.
Tracey Deiss, DVM, is Zoetis’s medical lead for feline pain and anxiety, as well as a general veterinary practitioner who earned her degree in veterinary medicine from Texas A&M University. In her free time, Dr. Deiss provides relief veterinary services to several clinics and is on the board of two veterinary medical organizations.
Have a question for us? Email efavilla@forbes.com with the subject line “Pet Peeves.”
This post was originally published on this site be sure to check out more of their content.